Revenue Growth & Enjoyment
Revenue Growth & Enjoyment
Earn more. See Fewer Patients. Enjoy Dentistry More.
This ebook is a must-read for Dental Practice Owners...
Get instant access to the Practice PIVOT Ebook where Dr. Tarun Agarwal breaks down the top 9 tips you need to implement into your practice TODAY if you want to grow your practice in 2023.
FEATURED EVENT
3D Summit 2024
This event is the go-to event if you want to grow your Dental Practice in 2024.
This year’s summit was so good that over half of our tickets for 2024 are already sold out to people who attended the 2023 summit – so get them while they’re still available!
We are going to have 6 industry experts at the event teaching, and you will walk away with REAL, PRACTICAL ACTION-STEPS to grow your practice in 2024!




Online Learning:

ExoCad Mastery
Master Exocad With Step-By-Step Video Lessons. Learn To Create Flippers, Surgical Guides, Dentures, And More With ExoCad.
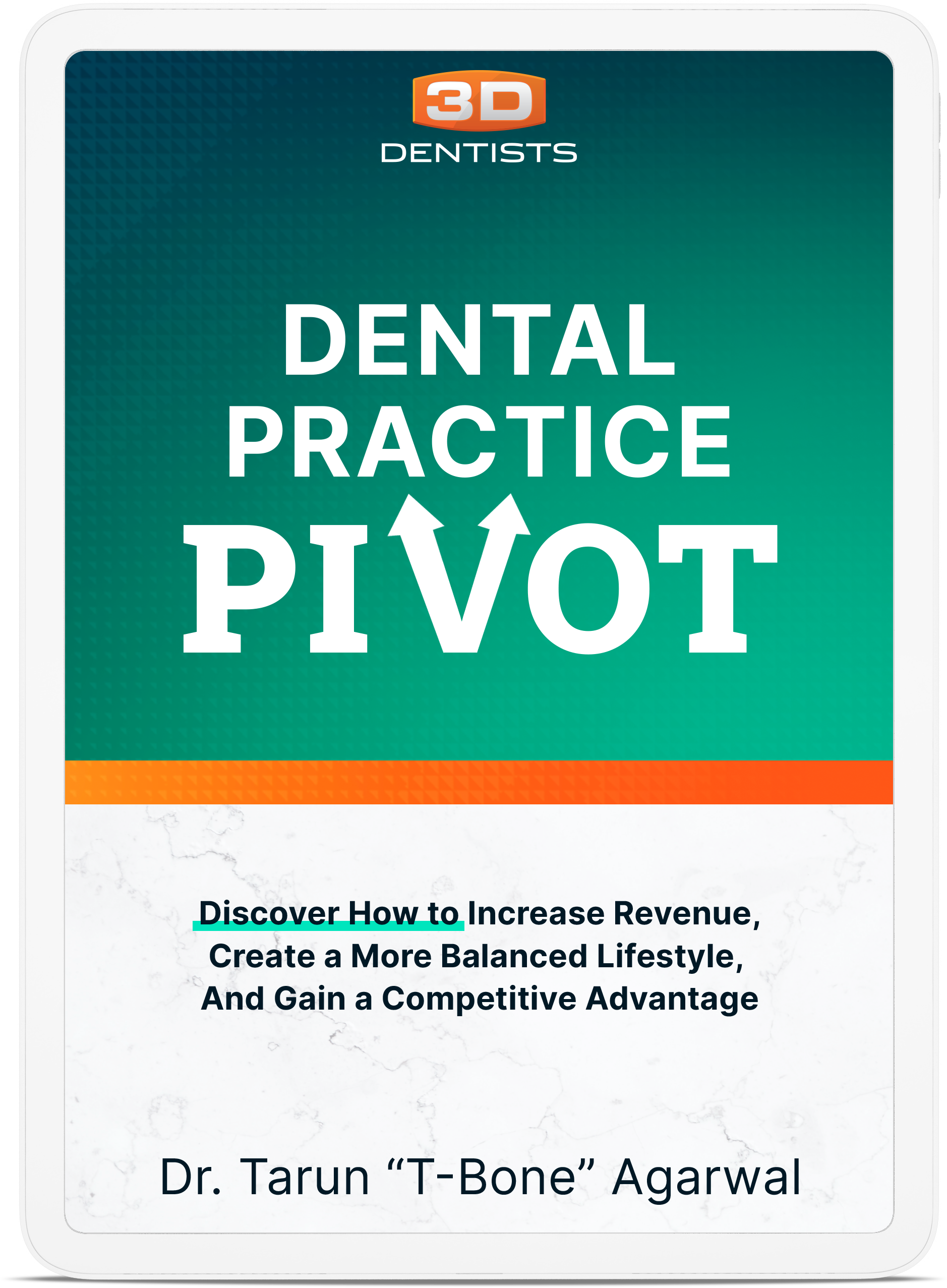
Case Acceptance 101
Master Exocad With Step-By-Step Video Lessons. Learn To Create Flippers, Surgical Guides, Dentures, And More With ExoCad.

Sleep Apnea Implementation
Slow Down To Speed Up. Dedicated to developing business principles and a case acceptance workflow that leads to YES!
Not sure where to start? We've got you.
We’ve mapped out a proven success path with our programs to help you get maximum benefit from all 3D Dentists has to offer.
Meet Your 3D Guides.
Each 3D Instructor is dedicated to teaching the clinical concepts and business strategies you need to succeed in dentistry. Not only are they recognized subject experts, they are practicing dentists who understand and feel the same struggles and challenges you face on a daily basis.

Dr. Tarun Agarwal

Dr. Sully Sullivan

Dr. Joc Jernigan

Dr. Timothy Anderson

Dr. Matt Standridge

Dr. Erin Elliott

Dr. Tarun Agarwal

Dr. Sully Sullivan

Dr. Joc Jernigan

Dr. Timothy Anderson

Dr. Matt Standridge

Dr. Erin Elliott
PODCASTS
Listen and learn.
Insightful conversations with successful dental professionals, industry experts, and so much more. Our podcasts reveal powerful stories, proven strategies, and secrets for thriving in the modern dental practice. Be sure to subscribe so you don’t miss an episode.


Making real change happen. For real people.

A message from the founder.
My promise to you — everything taught at our educational events is based on experience from everyday general practice and my personal journey in practice growth and development. You and I face the same challenges. I am a practice owner and a full-time practicing dentist.
You’ll love the down to earth atmosphere and practical approach to dentistry.
Dr. Tarun Agarwal